I don't know about you, but I never expect to be one of
those people. You know, the people who are suddenly faced with
really unexpected or
really sucky or
really hard things, smack in the face: suddenly nose-to-nose with
scary and
ugly and
hard in real life. No rewind. No clicking away from a blog or news article. No hanging up the phone. No promising to pray for the sudden catastrophe in someone else's life. This is
my life now. I've never been one of those people, never thought I would be.
It has taken me awhile to get to the point where I can view the last week and a half more through the lens of miraculous, overwhelming, grace-filled mercy from God, rather than being blindsided by a frightening, completely unexpected, heartbreaking diagnosis for our baby girl. Maybe heartbreaking is too strong a word. I know it broke my heart.
I'm one of those crazy people who started researching babies and birth and maternity care providers long before we were ready to start a family. I started taking prenatal vitamins, like, a year ago, just to be safe. And Elaina's
19-week ultrasound was completely, perfectly normal: Fingers and toes and organs all being beautifully knit together. Other than a lot of nausea, it's been a pretty textbook pregnancy.
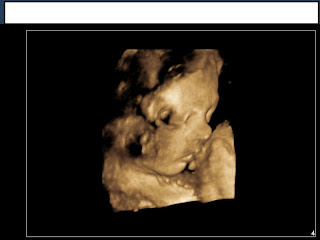
Before losing my job last November, I was a cardiac sonographer {specialist who uses ultrasound to look at people's hearts} for five years. I know a lot of people in the ultrasound industry. When I was 13 or 14 weeks pregnant, one of my college classmates told me about an opportunity to get a free ultrasound. She works for an ultrasound manufacturing company and they are always in need of "models" {read: anybody who's willing} to test new ultrasound systems. We decided to wait because at that point, babies just look like little aliens and it can be kind of freaky. Life got busy, I forgot for a few months, and then a couple weeks ago she emailed me and we set up a time for the ultrasound.
We went in on Friday of last week, just a few days after deciding that Miss Peanut's name is Elaina. I was 30 weeks pregnant; we had one birth class left to go; and after a completely normal ultrasound in February, we were expecting nothing more than to enjoy seeing our daughter swim around. Instead, we discovered a mass in Lainie's chest. Otherwise she appeared perfectly healthy. We left with heavy hearts, knowing that we needed to contact our midwife on Monday and get an "official" ultrasound.
It was a really weird weekend...with a deep, unspoken undercurrent that something big is "off." I did some online research on chest masses, but quickly realized that was a bad idea and stopped. We decided to tell our families and close friends so they could pray. We kept doing the normal things we'd planned: garage sales, replacing the brakes on my car, Sunday afternoon at Babies 'R' Us and Ikea to buy baby stuff. If that isn't bizarre: Our first-ever trip to Babies 'R' Us, choosing a carseat and stroller and evaluating crib mattresses, and this nagging cloud always overhead that there's something wrong with our baby's chest...something we would not have known about had I not had ultrasound connections, had we not made the time to get this ultrasound "just for fun"...
We got in for an official ultrasound on Monday afternoon. The doctor was pretty confident that the mass was a harmless cystic structure--nothing to worry about, sometimes they even disappear before birth. Mike and I were ecstatic. Even if it didn't disappear and our baby eventually needed surgery to remove it,
that was not a big deal compared to some of the other things it could have been. We could do this. This was really, really good news.
Tuesday morning, one of the midwives called me. She had asked another doctor to look at the ultrasound, and this doctor thought the mass might indicate a diaphragmatic hernia--a hole in the diaphragm {the muscle separating abdomen from chest} that lets abdominal organs go up into the chest. She wanted to schedule us for another ultrasound at a high-risk pregnancy clinic. Of course I said yes. Then I called Mike, told him, and cried. Wednesday morning my ladies' Bible study prayed for us. I'd barely gotten home when the high-risk clinic called to schedule the ultrasound and a consult with a perinatologist for the next morning at 8 AM. That was a relief--I'd expected a long wait to get in.
I prepared an arsenal of questions for the perinatologist: technical questions, anatomical questions, everything. Retrospectively, I think I wanted to convince her that the mass wasn't a diaphragmatic hernia. When she came in the consultation room after the ultrasound and gently told us to forget everything the other doctor had said about a cyst, that this is definitely a hernia--
BAM.
We are
those people.
No longer
normal
low-risk pregnancy
healthy baby
midwife
birth center
home a few hours after birth
Now we are
high-risk
follow-up ultrasounds
fetal echo
cardiology consultation
surgery consultation
perinatology consultation
delivery at the university hospital
ventilator
Children's Hospital
"you might
be able to touch her after she's born, if she's stable enough"
surgery on my newborn
weeks in the NICU
a host of possible complications, some long-term
There are still so many things we won't know until our slew of tests and consultations at Children's Hospital two weeks from now. Even then, I know that many of our questions are of the "we won't know 'til she's born" variety:
Can we hold her? Will she definitely need respiratory support? How often do these babies need long-term help breathing? Have long-term gastrointestinal problems? Will she be able to learn how to nurse and swallow? How soon will they do surgery? How long will she probably have to stay at the hospital?
Here is what we do know. The diaphragm, the sheetlike muscle that separates abdominal cavity from chest cavity and is vital for breathing, forms in the second month. A diaphragmatic hernia occurs when there is a hole in the muscle and abdominal organs move into the chest. This compromises lung development and, because the diaphragm functions in breathing and has a hole in it, breathing is affected. The hernia must be surgically repaired as soon after birth as possible.
In Lainie's case, the hole is probably small, because no abdominal organs were seen in the chest at her 19-week ultrasound. That is actually a good thing. Even now, only part of her stomach and a tiny bit of intestines are in her chest--with larger hernias the liver, spleen, entire stomach, and bowels may be in the chest. Her left lung is compressed because of this, but her heart is only shifted a tiny bit from where it should be. Again--good. And everything else about her is perfectly normal: swallowing, suckling, moving, practice breathing. At this point, the perinatologist described this as a "best case hernia." She will be closely monitored, of course, because things can change.
Slowly, my perspective is shifting. There is still grief, a lot of grief. I don't want my tiny, fresh, new little baby to be cut open. I don't want to be separated from her. I don't want her to need machines to help her breathe. I don't know what life will look like after she's born, short- or long-term. Part of me wants her to stay inside, safe and cozy, because everything is fine as long as she's there. It's when she comes out and has to breath on her own that all hell breaks loose {at least that's what it seems like to me}.
But I'm beginning to see God's incredible grace woven throughout this story:
If you have a normal ultrasound at 18-20 weeks, you don't normally get another one. There's no need.
Yet I
just happen to have a friend who got us an ultrasound at 30 weeks, "just for fun."
If Lainie, with an undetected diaphragmatic hernia and resultant underdeveloped lungs, had been born outside a hospital that could give her advanced respiratory support, the outcome could have been really bad.
Yet our midwife asked a perinatologist for a second opinion, even though the doctor who interpreted the ultrasound was quite certain the mass was a harmless cyst.
The fact that this was found and correctly diagnosed, period?
A miracle.
The fact that we live less than 25 miles from nationally-recognized hospitals that care for 15-20 babies with diaphragmatic hernias per year? We don't have to drive for hours, or move, in order for Lainie to get top-notch care.
The fact that this is a small hernia and doesn't appear to be negatively impacting her other organ systems? Praise the Lord!!
That's what Mike kept saying as we drove home, fresh with the diagnosis: "Praise the Lord that this was found! Praise the Lord that _______ wanted to do the free ultrasound for you! Praise the Lord that we didn't do the ultrasound earlier, before the hernia showed up! Praise the Lord that this is fixable! Praise the Lord that this is a 'good' hernia!"
Yes,
praise the Lord.